Koetting
Koetting
GLAUCOMA
What is glaucoma?
Glaucoma is a group of diseases causing damage and deterioration to the optic nerve. It is the leading cause of blindness in people over 40 years old. Fortunately, today, glaucoma treatments are better than ever. The optic nerve is the cable that carries information about what your eyes see to the brain where it is processed. In most glaucoma cases, fluid inside the eye builds up causing an increase in intraocular pressure. While it is not fully understood, it is thought that this increase in pressure damages the individual nerve fibers within the optic nerve. When left untreated this damage progresses over time and can lead to blindness.
Types of glaucoma
There are two main categories of glaucomas: open-angle glaucoma and angle-closure glaucoma.
Open-angle glaucoma is the most common type of glaucoma. It is classified by a buildup of fluid likely due to a clogged or poorly functioning drainage angle (called the trabecular meshwork). This type of glaucoma has previously been termed a “silent blinder” as it is painless and causes no visual symptoms at first. Open-angle glaucoma is usually diagnosed during routine eye health examinations.
Angle-closure glaucoma is less common than open-angle glaucoma. In this condition, pressure inside the eye spikes because the drainage angle becomes very narrow or closed, blocking fluid from leaving the eye. When the drainage angle closes, intraocular pressure can rise quickly, which makes this condition an emergency. Unlike open-angle glaucoma, acute angle-closure glaucoma can produce symptoms of redness, pain, light sensitivity, nausea, and blurred vision.
Risk factor
In general, glaucoma impacts about one percent of the world’s population. There are several known risk factors for glaucoma. These include:
- Age over 40
· Race of African American, Hispanic, or Asian
- Positive family history
- High eye pressure
- History of eye injury
- Having thin corneas
- Being nearsighted or farsighted
Diagnosis
To diagnose glaucoma, a doctor will order several tests to evaluate your risk. The first test done will be to measure your eye pressure. While glaucoma is correlated to having high eye pressure, some patients with normal eye pressure may also develop glaucoma. Other tests include a threshold visual field, pachymetry to measure corneal thickness, optical coherence tomography laser (OCT) scanning of the optic nerve, and a dilated eye exam to assess any glaucoma-like changes to the optic nerve. Once all this data is collected, the doctor will evaluate these tests together to determine a risk and proper treatment.
Symptoms of glaucoma
There are usually no symptoms of high eye pressure, which is why regular eye exams are so important. In advanced glaucoma patients may notice a reduction in peripheral vision, progressing to tunnel vision. Acute open-angle glaucoma has additional symptoms of redness, pain, nausea, light sensitivity, and blurred vision.
Treatments
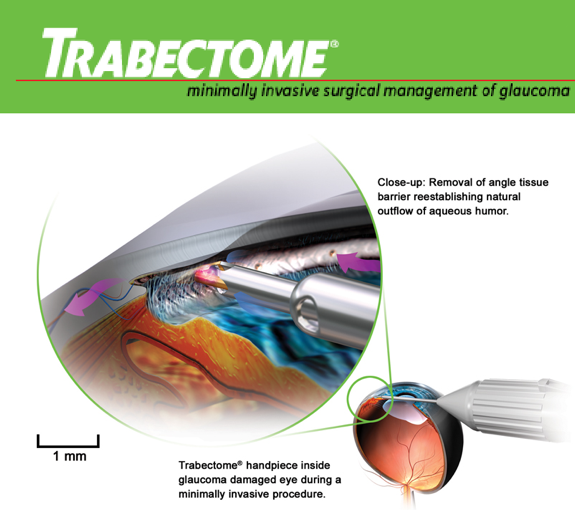
Treatment for glaucoma is catered to lowering the intraocular pressure. Once glaucoma is diagnosed, a personalized treatment plan will be established for every patient, based on the type and severity of the condition. Glaucoma may be treated with eye drops, laser and conventional surgery, or both. Eye drops are the most common management for glaucoma, as they generally do a very good job of lowering the eye pressure. In patients who struggle with instillation of drops or who aren’t getting the necessary pressure lowering effects, surgery may be indicated. Laser surgeries are simple, minimally invasive procedures done on an outpatient basis and have a low risk of side effects. In cased of advanced glaucoma, conventional surgical methods may be necessary. These procedures create a new drainage channel for aqueous fluid to leave the eye.
Many surgeons are now performing a new group of glaucoma surgeries, called minimally invasive glaucoma surgery (MIGS). This is done in conjunction with cataract surgery and involves a stent being carefully placed in the drainage angle to allow passage of aqueous fluid. These stents can help to lower eye pressure and may reduce the number of drops patients are taking.
Our doctors use all the most recent diagnostic equipment and are well-educated on the advancements in glaucoma treatment. Schedule an appointment to speak with one of our doctors about your options.
Laser Assisted Cataract Surgery
A cataract is a clouding of the naturally clear lens inside the eye. The development of cataracts is a normal part of the aging process and usually takes place over the course of several years.
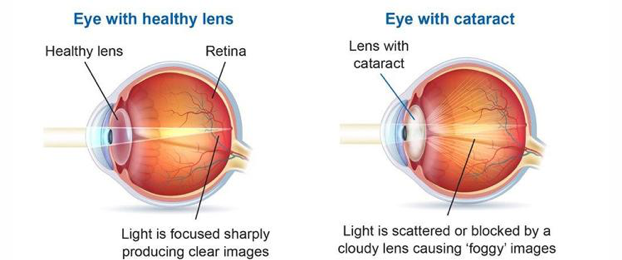
As cataracts develop and the lens clouds, you may experience a reduction in vision. This includes blurred vision, difficulty driving at night, glare, halos, needing more light to read, poor color vision, and reduced contrast sensitivity. Adjustments in glasses and contact lens prescriptions can be made to improve vision in early stages. Eventually, as the cataract progresses, changes in prescription will not help to improve vision. Surgical removal of the cataracts is indicated when the reduction in vision is impacting quality of life.
At The Koetting Associates Eye Center, we have co-managed thousands of cataract surgeries. We work only with the most experienced surgeons offering the latest in laser assisted cataract surgery. The introduction of the Femtosecond laser has made cataract surgery more accurate, more repeatable, and safer than ever before.
Cataracts are treated by removal of the cloudy lens and replacement with an artificial lens, called an intraocular lens implant. With today’s technology, there are several intraocular lens implants offered to fit you best. Implant options include standard lenses, multi-focal lenses, accommodating lenses, and toric lenses (astigmatism correcting). After extensive testing, the doctor will recommend a lens that best fits your needs.
Patient’s often ask if it they can continue to wear their glasses or contact lenses after the procedure. The short answer is, absolutely. While the surgeon’s goal is to implant a replacement lens to match your prescription, many patients still benefit from using glasses or contact lenses to sharpen their vision. It is often encouraged for patients to resume glasses or contact lens wear after surgery to maximize their vision potential following the cataract surgery.
A new protocol in cataract surgery becoming more popular is dropless cataract surgery. Until recently, post-operative care involved a month-long eye drop regimen. These drops help to ensure a smooth, safe recovery from the surgery. For some patients, drops may be time consuming, difficult to instill, and expensive. Dropless cataract surgery is achieved by injecting a compound medication into the eye directly following cataract surgery while the patient is still under anesthesia. This compound medication will contain most or all of the medications typically prescribed in drop form after surgery. Talk to one of our doctors at The Koetting Associates Eye Center today about how you could benefit from this new approach to cataract surgery.
Keratoconus
The clear front surface of the eye is called the cornea and is responsible for focusing light to the back of the eye. Keratoconus is a condition that causes a thinning and forward bulging of the cornea, affecting one’s ability to focus light and see properly. A study in the Netherlands found the number of people living with the disease to be as high as 1 in 375. Keratoconus typically begins to cause changes to the cornea in the teens, is most often diagnosed in the 20’s, and progresses through the early 40’s. As the disease progresses, eye glasses no longer provide satisfactory vision and specialty contact lenses are required. Specialty contact lenses, such as scleral lenses, recreate a smooth surface to the front of the eye so light can focus again. Advancements in technology allow us to diagnose keratoconus at an earlier age. Treatment options have also dramatically improved in the recent years, so early detection and intervention are more important than ever.
Causes of Keratoconus
Despite significant research, not a lot is known about exactly what causes keratoconus. Some research suggests that it is a genetic condition and can be passed down to family members. Those that have keratoconus have excessive enzymes that breakdown and weaken the collagen fibers in the cornea, allowing it to protrude forward. Family members of those with keratoconus are at higher risk of having too much of this enzyme.
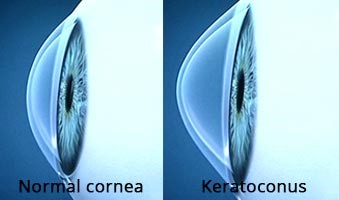
Others associate keratoconus with allergic conditions such as chronic allergies and eczema. Vigorous eye rubbing that is common in patients with allergic conditions can also weaken the fibers in the cornea that allow it to keep is round shape. For this reason, those who have been diagnosed with or those with high-risk for keratoconus should avoid excessive eye rubbing.
Connective-tissue disorders have been linked to an increased risk of keratoconus as they can cause weakening of the connective tissue within the cornea. Examples include Ehlers-Danlos syndrome, osteogenesis imperfecta, mitral valve prolapse, Marfan syndrome, etc.
Symptoms of Keratoconus
Symptoms of keratoconus are often first experienced in the late teens and worsen as the condition progresses. Symptoms vary but often include:
- Blurry vision
- Distorted vision
- Nighttime glare
- Nearsighted and astigmatism
- Poor vision with new glasses
- Frequent prescription changes
- Poor vision with soft contact lenses
- Discomfort with contact lenses
How is Keratoconus Diagnosed?
There are a handful of diagnostic tests and procedures that can aid in the diagnosis of keratoconus. While corneal mapping is essential to confirm the diagnosis, all the following tests are useful as they provide information on the severity and long-term outcome of the disease.
Refraction: A procedure done to determine a glasses or contact lens prescription, and monitor changes to these prescriptions over time.
Slit Lamp Examination: A specially designed, high-powered, microscope is used by an eye care professional to visualize the front surface of the eye and examine all layers of the cornea related to keratoconus.
Corneal mapping: Also known as corneal topography, corneal mapping scans the front surface of the eye and creates an elevation map of the cornea. It also highlights areas that have excessive curvature, which is characteristic of keratoconus.
Corneal thickness measurements: The thickness of the cornea can be measured with a scanning laser or ultrasound technology and compared over time. Progressive corneal thinning can be an indication of keratoconus.
Rigid Lens Acuity Test: A rigid surface contact lens is applied to the surface of the eye. If the patients vision improves compared to their glasses prescription, they may have an irregular cornea because of keratoconus.
Treatment for Keratoconus
In the early stages, keratoconus can be treated with glasses and soft contact lenses. As the disease progresses and the cornea becomes more irregular, rigid contact lenses become the mainstay treatment. Most patients with keratoconus do not progress beyond this point. However, some patients continue to advance to corneal thinning and scarring that does not correct well with contact lenses and a corneal transplant is needed.
Specialty contact lenses options include:
Custom soft contact lenses: Mild to moderate keratoconus can be managed with custom soft contact lenses. Today’s technology allows for the manufacturing of specialty soft contact lenses with virtually any prescription.
Rigid gas permeable contact lenses (RGPs): Commonly referred to as hard lenses, RGPs are an excellent choice for mild to moderate keratoconus. Typically, they provide better vision than soft lenses as they can reshape the irregular surface of the cornea created by keratoconus. As the keratoconus progresses, it may become difficult to maintain proper lens fit and keep the lens from falling off the eye because of its relative small size. Contact lens comfort can also become an issue.
Piggyback contact lenses: A small diameter hard contact lens is worn over a soft contact lens. This contact lens fitting design has the visual benefits hard lenses and the comfort of soft contact lenses.
Hybrid contact lenses: These lenses have a hard contact lens center attached to a soft contact lens skirt. As in piggyback lenses, hybrid contact lenses are designed to provide the vision of hard lenses with the comfort of soft contact lenses. Advancements in hybrid contact lens technology now allows for the fitting of all stages of keratoconus.
Scleral contact lenses: These are large diameter hard contact lenses that provide clear and comfortable vision. Scleral contact lenses are unique in that they never touch the cornea. They vault over the cornea and gently rest of the white part of the eye, or sclera, as their name implies. Scleral lenses tend to be very comfortable and stable on the surface of the eye because of their large size. They are available in a variety of shapes and sizes, meeting the needs of “normal” eyes all the way to severe keratoconus or corneal transplants.
Surgical Treatment for Keratoconus
Keratoconus surgical procedures do not eliminate the need for specialty contact lenses. While it may be easier to wear contact lenses after surgery, most of the time they will still be required to achieve optimal vision.
Collagen cross-linking (CXL): Until the advent of collagen cross-linking, surgery for keratoconus usually meant a corneal transplant. This was a last resort because of the associated complications. These patients were fit with specialty contact lenses until vision was no longer satisfactory and a corneal transplant was necessary to maintain quality of life. Today, collagen cross-linking should be considered a first-line therapy in patients with progressive keratoconus.
Although collagen cross-linking has been around for over a decade in other countries, it was not FDA approved in the United States until 2016. As keratoconus progresses it thins and weakens the cornea, which over time causes it to bulge forward. Collagen cross-linking is a minimally invasive procedure is performed to strengthen the cornea and arrest these changes. This may improve vision in some patients and lessen the likelihood of a future corneal transplant.
Collagen cross-linking is performed with riboflavin (vitamin B2) eye drops and ultraviolet light. The procedure is done one of two ways: epithelial-on or epithelial-off. Typically, epithelial-on takes longer to perform but is associated with fewer complications.
Intacs: Originally introduced to correct low amounts of nearsightedness, intacs are now used to treat irregular corneal surfaces, such as keratoconus. They are surgically implanted into the outer edge of the cornea to flatten and create a more regular surface. These are of similar material to rigid contact lenses and cataract surgery implants. In patients with keratoconus, intacs can make it easier to tolerate contact lens wear and improve the vision with glasses. Some surgeons are finding success coupling collagen cross-linking and intacs in one procedure. To achieve the best vision possible, specialty contact lenses are still required by almost all patients with keratoconus.
Corneal transplantation: When corneal scarring from keratoconus causes vision loss this is not correctable with specialty contact lenses or glasses and a corneal transplant may be necessary. In this procedure, the diseased cornea is surgically replaced with a healthy donor cornea. Corneal transplants are performed a variety of ways, from a partial thickness to a full thickness transplant. Depending on the procedure, the healing process varies among patients, ranging from a few weeks to a year or more. The most appropriate corneal transplant procedure will be determined on an individual basis.
Although corneal transplantation is a relatively safe procedure, there are serious risks that need to be considered before the procedure is performed. Graft rejection is a complication that occurs when the body’s own immune system attacks the donor cornea. This has been reported in 10% of corneal transplants and requires steroid eye drops or a second transplant. It is always best to first attempt to improve vision with specialty contact lenses before a corneal transplant to minimize risks of complications.
Please call Koetting Eye Center today to schedule a consultation with one of our keratoconus specialists.
Corneal Reshaping with Orthokeratology
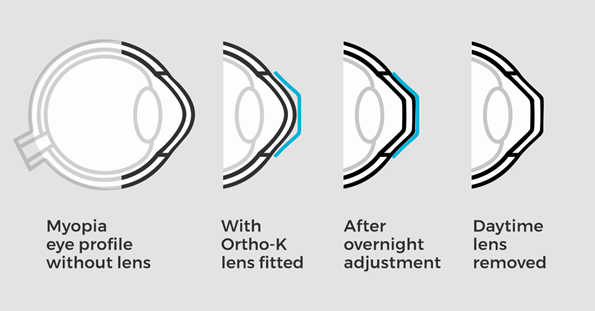
Imagine wearing a contact lens while you sleep and removing it in the morning to enjoy clear, comfortable vision the rest of the day. Orthokeratology, or ortho-k, uses a specially designed rigid gas permeable contact lens that gently reshapes the front surface of the eye while you sleep. This safe and effective treatment is a great alternative to LASIK for those who do not want the risk or expense of surgery.
How Does Ortho-K work?
When a person cannot see clearly, it is because their eye is too long, too short or the surface is misshaped. Images appear blurred because they fail to focus on the retina (back surface of the eye). To create an ortho-k lens, the front surface of the eye is mapped using a high-tech instrument called a topographer. This allows the doctor to create a specially designed ortho-k lens to address the patient’s unique vision problem. The lens is then manufactured from a highly oxygen permeable material which allows the eye to breathe overnight and maintain excellent health. This corneal reshaping lens has multiple specialized curves that gently reshape the front of the eye and allow it to focus sharp images on the retina. The result is clear, crisp vision upon awaking and removing the lens.
Who is a Candidate for Ortho-K?
Using today’s technology, we can correct low to moderate amounts of nearsightedness and astigmatism. Some patients are even candidates to have their presbyopia corrected, which would minimize or eliminate their dependency for reading glasses.
How Long Does Ortho-K Last?
Corneal reshaping typically last 2-3 days, or longer. It depends on the amount of nearsightedness initially corrected. The more nearsighted the patient was starting out, the quicker the cornea reverts to its original shape. It is usually advised to wear ortho-k lenses nightly.
Why Ortho-K?
Individuals physically active will benefit the most from corneal reshaping. Sport goggles are cumbersome and can negatively affect athletic performance. Contact lenses can dry up and fall out during physical activity. Water sports can be especially challenging with prescription goggles or contact lenses. Orthokeratology addresses these concerns and allows for peak physical performance without the distraction of goggles or contact lenses.

Certain contact lenses can disrupt the tears as they spread over the surface of the eye, causing them to evaporate quickly. This results in symptoms of dry eye and fluctuating vision. Patients fit with ortho-k contact lenses will not experience these contact lens related problems. Also, these patients are less likely to have eye infections or irritation from airborne particles getting behind their contact lenses. Therefore, ortho-k is ideal for anyone who spends a lot of time outside, in dusty environments or are prone to allergies.
Children and Ortho-K
Children diagnosed with nearsightedness are the best candidates for corneal reshaping. In addition to the previously mentioned benefits of a glasses and contact lens free lifestyle, which is especially important for children, ortho-k may slow the progression of nearsightedness in children (myopia control). There are multiple sight threatening complications of being highly nearsighted; such as, glaucoma, macular degeneration and retinal detachments. The risk of theses complications later in life can be lessened by reducing nearsightedness in adolescence. To learn more, visit Myopia Control and Kids.
Corneal Refractive Therapy (CRT)
While there are various orthokeratology lens options available, the doctors at The Koetting Associates utilize a proprietary fitting technique called Corneal Refractive Therapy (CRT). Doctors who fit CRT ortho-k lenses are required to complete a training and certification process. Theses lenses are carefully designed to provide patients with excellent vision and a consistent lens fit. CRT ortho-k lenses have been the gold standard in corneal reshaping for many years.
Please call today to schedule a consultation with one of your orthokeratology certified doctors!
Brentwood:
2511 South Brentwood Blvd.
St. Louis, Missouri 63144
(314) 863-0000
Ellisville:
113 Old State Road Suite 101
Ellisville, Missouri 63021
(636) 256-7800